Naltrexone for Opioid Use Disorder: A Guide
1. Introduction: How Naltrexone Helps with Opioid Use Disorder (OUD)
If you've made the brave decision to stop using opioids, you know the journey doesn't end after detox. Naltrexone is a non-addictive medication that can be a powerful ally in helping you stay in recovery and reclaim your life. It works as an opioid antagonist, meaning it completely blocks the effects of opioid drugs in the brain.¹ This makes it a powerful tool for preventing relapse. Unlike opioid-based treatments like methadone or buprenorphine, naltrexone itself does not activate the brain's opioid receptors, so it does not cause physical dependence or withdrawal symptoms when stopped.¹ This key difference offers a treatment path for OUD that is free from opioid medication.
The primary role of naltrexone in OUD treatment is to help individuals who have already stopped using opioids to stay opioid-free.¹ By blocking the euphoric "high," it removes the primary incentive for opioid use, which can significantly reduce cravings and help break the cycle of relapse.
It is crucial to understand that naltrexone is not a standalone cure for OUD. It is most effective when integrated into a comprehensive treatment program that includes counseling, behavioral therapy, and participation in support groups like Narcotics Anonymous (NA) or SMART Recovery.⁵ This holistic approach addresses the psychological and social aspects of addiction, providing the support necessary for lasting recovery.
2. How Naltrexone Works: The Science Behind Blocking Opioid Effects
Naltrexone's mechanism for treating OUD is direct and powerful. It works by binding very tightly to the opioid receptors in the brain and throughout the body.² By occupying these receptors, it acts as a shield, effectively blocking other opioid molecules—such as those from heroin, fentanyl, or prescription painkillers—from attaching and producing their effects.¹
When a person with naltrexone in their system uses an opioid, they will not experience the rush of euphoria or the pain-relieving effects they expect. This action fundamentally breaks the connection between using the drug and feeling the reward.¹ Over time, this helps to extinguish the learned behaviors and cravings associated with opioid use. Because the "reward" is gone, the motivation to use opioids diminishes significantly.
This makes naltrexone different from other primary OUD medications. Buprenorphine (Suboxone) is a partial agonistthat provides some opioid effect to reduce withdrawal and cravings, while methadone is a full agonist that does the same more potently. Naltrexone, as an antagonist, provides no opioid effect at all.¹ It simply blocks the path for other opioids. This "blockade" approach is ideal for individuals who are highly motivated to live a life completely free from all opioid substances.
This short video explains the science behind Naltrexone for OUD:
3. Who Can Benefit from Naltrexone? Patient Selection and The Opioid-Free Challenge

Naltrexone is a valuable option for specific individuals with OUD. The ideal candidates are people who are highly motivated to achieve total abstinence and have successfully completed a full detoxification from all opioids.¹⁷ Because naltrexone will cause severe, immediate withdrawal if taken while opioids are still in the body, a mandatory opioid-free period of 7 to 14 days is required before starting treatment.⁹ This is the single most important criterion for patient selection.
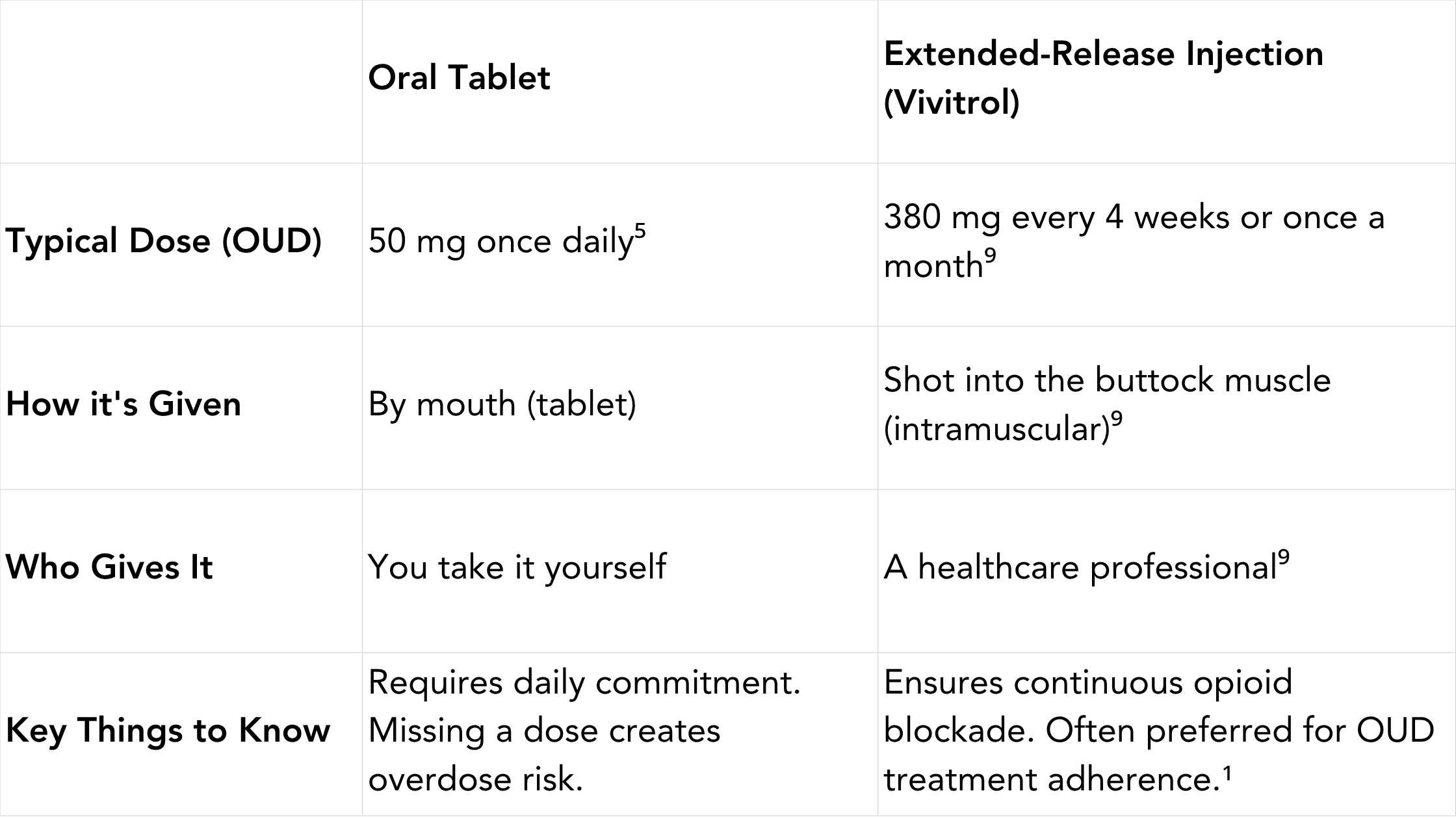
Naltrexone is available in two forms: a daily oral tablet and a long-acting monthly injection sold under the brand name Vivitrol.
- Oral Naltrexone (Pill): The typical dose is 50 mg taken once a day.⁵ While effective, it requires the commitment of taking a pill every day. Forgetting a dose can leave a person vulnerable to relapse and overdose.
- Injectable Naltrexone (Vivitrol): Vivitrol is a 380 mg injection administered by a healthcare professional once every four weeks.⁹ This long-acting formulation is often preferred for OUD treatment because it removes the burden of daily dosing, ensures continuous opioid blockade, and can significantly improve treatment adherence.¹
The choice between the oral pill and the monthly shot depends on individual circumstances. Vivitrol is often recommended for those who struggle with medication adherence or prefer the convenience of a once-a-month treatment.
The absolute necessity of completing detox is a major consideration. This process can be physically and emotionally challenging, and often requires medical supervision. Before starting naltrexone, a healthcare provider will typically perform a urine drug screen and may use a naloxone challenge test to ensure no opioids are present in your system.¹⁹ This rigorous screening process is vital for your safety and highlights that naltrexone is best suited for individuals who are stable in their early recovery and committed to maintaining abstinence.
4. Effectiveness and Benefits: What the Research Shows
Multiple studies have demonstrated naltrexone's effectiveness in supporting recovery from Opioid Use Disorder, primarily by preventing relapse. When used correctly, naltrexone has been shown to significantly increase the time people remain opioid-free compared to a placebo.²
For the injectable form, Vivitrol, research is particularly strong. One landmark study found that patients with OUD who received monthly Vivitrol injections were much more likely to remain abstinent and avoid relapse over a 24-week period compared to those receiving a placebo.² People treated with Vivitrol also reported fewer opioid cravings and were able to stay in treatment longer.¹
While naltrexone is highly effective at blocking opioids, it is important to compare it to other MAT options. Buprenorphine and methadone are often easier for patients to start because they do not require a full detox period; in fact, they are used to manage withdrawal. For many, these agonist therapies are a more accessible first step.
However, naltrexone offers a distinct advantage for those who want to avoid taking any opioid-based medication. It provides a pathway to recovery without physical dependence on the treatment itself. The choice between naltrexone and agonist therapies is a personal one and should be made after a thorough discussion with a healthcare provider about your medical history, recovery goals, and ability to safely navigate the detox period.
5. Important Precautions and Potential Side Effects
While naltrexone is a safe medication for most people, understanding its risks and side effects is essential, especially for those with OUD.
The Two Most Critical Risks for OUD:
- Precipitated Opioid Withdrawal: This is an immediate, severe, and potentially dangerous withdrawal reaction that occurs if you take naltrexone while opioids are still in your system. Symptoms include intense nausea, vomiting, body aches, cramps, anxiety, and more. You must be opioid-free for 7-14 days before your first dose.
- Risk of Opioid Overdose: Naltrexone lowers your tolerance to opioids. If you stop taking naltrexone and then use opioids—even in an amount you previously tolerated—you are at an extremely high risk of a fatal overdose. This is because your body is no longer accustomed to the drug's effects. It is strongly recommended that you carry a medical alert card stating you are on naltrexone treatment.⁵
Common Side Effects of Naltrexone:
Side effects are generally mild and often improve over time. They include nausea, headache, dizziness, nervousness, fatigue, and difficulty sleeping.³ Taking the oral pill with food can help with stomach upset.
Serious Side Effects and When to Seek Medical Attention: Be sure to review the side effects possible with Naltrexone prior to taking this medication. Seek immediate medical attention if any serious symptoms occur.
- Liver Problems (Hepatotoxicity): Naltrexone can cause liver stress, especially at high doses. Your provider may monitor your liver function with blood tests. Watch for yellowing skin/eyes, dark urine, or persistent stomach pain.¹⁷
- Depression and Suicidal Thoughts: Report any sudden or severe changes in mood, behavior, or thoughts of self-harm to your doctor immediately.
- Injection Site Reactions (for Vivitrol): Seek immediate medical help for severe pain, swelling, blistering, lumps, or open wounds at the injection site.
- Allergic Reactions: Seek emergency help for hives, difficulty breathing, or swelling of the face, lips, or tongue.
6. Dosage and Administration: Pills You Take vs. Vivitrol Shot
Naltrexone is administered as either a daily oral tablet or a monthly intramuscular injection.
Duration of Treatment: The length of naltrexone treatment for OUD is personalized. It is generally recommended for at least several months to support early recovery, but many individuals benefit from long-term treatment to maintain abstinence and prevent relapse.⁶ The decision should be made in partnership with your healthcare provider based on your progress and recovery needs.
7. Drug Interactions and What to Avoid
Being transparent with your doctor about all medications and substances you use is critical for safety.
- Opioids: The most significant interaction. Naltrexone will block all opioid medications, including prescription painkillers (oxycodone, morphine), cough syrups with codeine, anti-diarrhea medications, and illicit drugs like heroin. Do not take them together.
- Other Medications: Naltrexone may interact with certain other drugs, such as disulfiram (used for AUD) and thioridazine (an antipsychotic). Inform your doctor of all prescription and over-the-counter medications you take.⁴
Naltrexone should not be used if you:
- Are currently using opioids or are physically dependent on them.
- Are in acute opioid withdrawal.
- Have acute hepatitis or liver failure.
- Have had an allergic reaction to naltrexone in the past.
8. Key Takeaways and Talking to Your Doctor
Naltrexone is a proven, non-addictive FDA-approved medication for preventing relapse in individuals with Opioid Use Disorder. By completely blocking the effects of opioids, it helps reduce cravings and supports long-term abstinence. It is available as a daily pill and, more commonly for OUD, as a once-monthly injection (Vivitrol) that ensures continuous protection.
The most critical safety consideration is the mandatory 7-14 day opioid-free period required before starting treatment to avoid severe precipitated withdrawal. Furthermore, the risk of a fatal overdose upon relapse after stopping naltrexone is extremely high due to lowered tolerance.
Naltrexone is an excellent option for highly motivated individuals who have completed detox and desire a recovery path free from any opioid-based medication. However, it is just one tool in a comprehensive treatment plan that must include counseling and support.
If you are considering naltrexone for OUD, an honest conversation with a healthcare professional is the essential first step. They can help you weigh the pros and cons, compare it to other MAT options like Suboxone, and determine if it is the safest and most effective choice for your personal recovery journey.
Works Cited
1. Naltrexone. SAMHSA. Accessed July 15, 2025. https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/naltrexone
2. How Does Naltrexone Work for Opioid and Alcohol Use Disorder? GoodRx. Accessed July 15, 2025. https://www.goodrx.com/naltrexone/naltrexone-alcohol-drug-addiction-treatment
3. Naltrexone Side Effects. Drugs.com. Accessed July 15, 2025. https://www.drugs.com/sfx/naltrexone-side-effects.html
4. Naltrexone Interactions. Drugs.com. Accessed July 15, 2025. https://www.drugs.com/drug-interactions/naltrexone.html
5. Naltrexone (Oral Route). Mayo Clinic. Accessed July 15, 2025. https://www.mayoclinic.org/drugs-supplements/naltrexone-oral-route/description/drg-20068408
6. Naltrexone for the Management of Opioid Use Disorder. American Family Physician. Accessed July 15, 2025. https://www.aafp.org/pubs/afp/issues/2018/1001/p450.html
7. Medication for Opioid Use Disorder. NIDA. Accessed July 15, 2025. https://nida.nih.gov/publications/research-reports/medications-to-treat-opioid-addiction/what-are-medications-to-treat-opioid-addiction
9. Naltrexone. Drugs.com. Accessed July 15, 2025. https://www.drugs.com/naltrexone.html
17. Chapter 4—Oral Naltrexone. Incorporating Alcohol Pharmacotherapies Into Medical Practice. NCBI. Accessed July 15, 2025. https://www.ncbi.nlm.nih.gov/books/NBK64041/
19. TIP 43: Medication-Assisted Treatment for Opioid Addiction in Opioid Treatment Programs. NCBI. Accessed July 15, 2025. https://www.ncbi.nlm.nih.gov/books/NBK64161/









-2.jpg)
.jpg)